500:
instigated by a mutation on the ferritin light chain polypeptide (FTL1) and was found to cause iron accumulation in the brain and neurodegeneration. Following the location of the first case of
Neuroferritinopathy, the majority of patients diagnosed with the disease have also been found in Northern and Northeast England. The localization of the majority of cases to Northern and Northeast England suggests that a common ancestor may be responsible for many or possibly all cases. Despite there being fewer than 100 cases reported and the disease's general location of Northern and Northeast England, many more cases of neuroferritinopathy have been diagnosed around the rest of the world in recent years.
61:
492:
213:, found in 7.5% of patients. Full control of upper limbs on the body generally remains until late onset of the disease. Over time, symptoms seen in a patient can change from one side of the body to the opposite side of the body, jumping from left to right or vice versa. Another route that the physically visible symptoms have been observed to take is the appearance, disappearance, and then reappearance once more of specific symptoms.
37:
209:. The symptoms accompanying neuroferritinopathy affecting movement are also progressive, becoming more generalized with time. Usually during the first ten years of onset of the disease only one or two limbs are directly affected. Distinctive symptoms of neuroferritinopathy are chorea, found in 50% of diagnosed patients, dystonia, found in 43% of patients, and
376:
343:(NBIA) disorders which share similar symptoms and imaging findings. Over time single-gene causes have been found for many NBIA disorders, like neuroferritinopathy. Before the availability of genetic testing, all such disorders were considered together and known as Hallervorden-Spatz syndrome, a term which is no longer used due to the
306:
subunits. In neuroferritinopathy, the gene encoding the light chain is mutated. Several different mutation variations have led to diagnosis as neuroferritinopathy; all of these mutations occur in the light chain. A mutated light chain is believed to inhibit ferritin's ability to effectively sequester
499:
Neuroferritinopathy was first discovered in 2001, with its first case being reported in
Cumbria from Northern England. The discovery of neuroferritinopathy was mediated by a study done on a large family suffering from a dominantly inherited basal ganglia disease. It was reported that the disease was
180:
Neuroferritinopathy is mainly seen in those who have reached late adulthood and is generally seen to slowly progress throughout many decades in a lifetime with the mean age of onset being 39 years old. A loss of cognition is generally only seen with late stages of the disease. Diagnosed patients are
131:
Treatment of neuroferritinopathy is focused on managing symptoms associated with chorea and dystonia using standard medications for each. The disorder is progressive and symptoms become worse with age. Fewer than 100 cases of neuroferritinopathy have been reported since its identification in 2001.
224:
Neuroferritinopathy results from abnormal brain iron accumulation. This iron accumulation is due to mutations in the FTL polypeptide, which is responsible for encoding proteins involved in iron metabolism. Neuroferritinopathy is most commonly caused by a single insertion of the nucleotide adenine
172:
and cerebellar cortices. Along with the accumulation of iron in the brain, neuroferritinopathy typically causes severe neuronal loss as well. Secondary symptoms may also arise. It is possible that the initial iron accumulation will cause additional neuronal damage and neuronal death. The damaged
310:
The concentration of iron in a healthy brain varies greatly from region to region. The specific regions of the brain that are associated with motor functions appear to have larger accumulations of iron than non-motor-related regions. This observation of varying iron concentrations is a possible
442:
Due to neuroferritinopathy's genetic etiology, the disorder is not currently curable. Furthermore, progression of the disorder cannot be effectively halted. Therefore current treatment focuses on managing symptoms of the disorder. No medication is available to treat all symptoms.
261:
functions to sequester and release iron, acting as an iron buffering system in cells. Iron is essential to brain function in oxygen transport and cellular metabolism for example. However, careful control of iron is important as increased brain iron levels catalyze the formation of
233:
varies by family. Neuroferritinopathy may also be caused by the insertion of two extra nucleotide bases. The insertion of bases into the L-chain ferritin gene causes the chain to lengthen and alter the sequence of the amino acids found in the gene, also known as a
351:, genetic systemic iron accumulation with neurologic features, and acquired diseases associated with iron excess or iron deficiency. Neuroferritinopathy is classified under the first category. Neuroferritinopathy is classified as a late-onset
1011:
412:
ferritin levels. However this is unreliable as method of diagnosis since some patients show typical serum ferritin levels even at the latest stages of neuroferritinopathy. Cerebral spinal fluid tests also are typically normal. Ferritin
123:
protein. Wild type ferritin functions as a buffer for iron, sequestering it and controlling its release. Thus, mutations in the light chain of ferritin result in the accumulation of iron in the brain which can be imaged using
387:
and other neuroimaging techniques. MRIs help identify the iron deposits in the cerebellum, basal ganglia, and motor cortex common to neuroferritinopathy. MRIs of affected individuals also show mild cerebellar and
433:
Genetic testing can confirm a neuroferritinopathy diagnosis. A diagnosis can be made by analyzing the protein sequences of affected individuals and comparing them to known neuroferritinopathy sequences.
249:, which have damaging effects to the brain. The iron accumulation characteristic of neuroferritinopathy particularly affects the cerebellum, basal ganglia, and motor cortex regions of the brain.
396:. Most importantly, the MRIs show misfolded ferritin proteins and iron deposits in the glial cells of the caudate, putamen, globus pallidus, cerebral cortex, thalamus, and
339:
Neuroferritinopathy was originally described with hallmark features of neurodegeneration and iron accumulation in the brain, leading it to be classified with other
348:
340:
327:, as iron accumulates in the brain over long periods of time. Neuroferritinopathy is diagnosed using either neuroimaging techniques, physiological tests, or
128:. Currently, neuroferritinopathy is the only neurodegenerative disease with an iron accumulation in the brain classified as an autosomal dominant syndrome.
173:
neurons may be replaced by other cells in an effort to reverse the neurodegeneration. These cells often have a higher iron content. The breakdown of the
144:
Neuroferritinopathy has several distinguishing signs and symptoms. These fall into two categories: diagnostic findings and physically visible symptoms.
408:
Blood tests usually come back normal in affected individuals so they do not serve as a reliable means of diagnosis. Blood tests can show low
1026:
906:
767:
674:
Zecca, L; Youdim, MB; Riederer, P; Connor, JR; Crichton, RR (November 2004). "Iron, brain ageing and neurodegenerative disorders".
1099:
245:, or programmed cell death. Accumulation of iron in the brain is extremely dangerous as excess iron catalyzes the formation of
177:
may also occur due to the loss of neurons and will subsequently allow more iron to access the brain and accumulate over time.
136:. Due to its genetic nature, current research is focused on therapeutic management of the symptoms caused by the disorder.
311:
explanation for the correlation between movement disorders and the iron imbalance within the central nervous system.
216:
While these symptoms are the classic indicators of neuroferritinopathy, symptoms will vary from patient to patient.
384:
508:
New potential treatment options being researched are
Venesection (removing red blood cells), Iron chelation with
241:
These mutations result in decreased iron-binding ability. The oxidative damage caused by increased iron leads to
630:
Chinnery, PF; Pagon, RA; Adam, MP; Ardinger, HH; Bird, TD; Dolan, CR; Fong, CT; Smith, RJH; Stephens, K (2010).
132:
Its incidence has been largely localized to
Northwest England, significantly in the Cumbria region suggesting a
1037:
791:
Batista-Nascimento, Liliana; Pimentel, Catarina; Andrade
Menezes, Regina; Rodrigues-Pousada, Claudina (2012).
160:. Patients who are diagnosed with neuroferritinopathy have abnormal iron accumulation in the brain within the
451:
shown to help with involuntary movements. Symptoms affecting movement (dystonia) have also been treated with
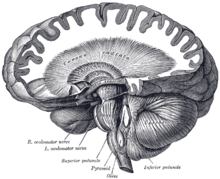
270:. These oxidative molecules can cause oxidative brain damage. Iron that is bound to ferritin in nonreactive.
181:
seen to retain most of their cognitive functioning until the most progressive stages of the illness sets in.
152:
Symptoms categorized as medically tested and diagnosed include iron accumulation in the brain, basal ganglia
414:
94:
1077:
324:
320:
97:
in nature, progress slowly and generally do not become apparent until adulthood. These symptoms include
307:
and hold iron. Without control of iron, it is free to cause oxidative brain damage as described above.
418:
417:
found in the skin, liver, kidney and muscle tissues may help in diagnosing neuroferritinopathy. More
364:
303:
202:
116:
112:
60:
267:
263:
235:
174:
871:
699:
206:
491:
319:
Neuroferritinopathy is primarily diagnosed in older adults, specifically in adults affected by
974:
912:
902:
863:
824:
773:
763:
691:
635:
603:
157:
74:
49:
964:
954:
894:
855:
814:
804:
755:
683:
595:
389:
586:
Lehn, A; Boyle, R; Brown, H; Airey, C; Mellick, G (September 2012). "Neuroferritinopathy".
444:
328:
246:
226:
367:(FTL) polypeptide gene while the fourth arises from a missense mutation in the FTL gene.
969:
942:
898:
819:
792:
759:
397:
133:
1093:
703:
599:
448:
409:
352:
82:
875:
581:
579:
577:
575:
573:
571:
569:
567:
565:
563:
561:
559:
557:
555:
553:
551:
549:
513:
456:
347:
ties of the namesakes. Brain iron disorders are now divided into three categories:
210:
90:
1042:
547:
545:
543:
541:
539:
537:
535:
533:
531:
529:
943:"Neurodegeneration with brain iron accumulation: update on pathogenic mechanisms"
741:
739:
737:
735:
733:
229:
end of the entire protein chain. However, exact location of the insertion in the
731:
729:
727:
725:
723:
721:
719:
717:
715:
713:
509:
355:
disease and is a dominantly inherited neurodegenerative disease. Four different
1020:
631:
472:
360:
344:
198:
153:
86:
959:
1048:
464:
460:
242:
109:
54:
978:
916:
867:
828:
777:
695:
639:
607:
809:
1072:
844:"Iron metabolism in the CNS: implications for neurodegenerative diseases"
468:
422:
258:
194:
169:
120:
102:
1003:
375:
393:
161:
1015:
480:
476:
452:
356:
190:
98:
859:
843:
687:
746:
Keogh, MJ; Morris, CM; Chinnery, PF (2013). "Neuroferritinopathy".
36:
1053:
893:. Handbook of Clinical Neurology. Vol. 120. pp. 851–64.
793:"Iron and Neurodegeneration: From Cellular Homeostasis to Disease"
490:
447:
has been shown to help with focal dystonia. The dopamine depleter
374:
1031:
936:
934:
932:
930:
928:
926:
625:
623:
621:
619:
617:
299:
230:
165:
78:
125:
225:
into the gene for L-chain ferritin which in turn, alters the
189:
Symptoms categorized as physically visible symptoms include
359:
are responsible for neuroferritinopathy. Three arise from
392:, or tissue breakdown, and gas cavity formation in the
349:
genetic neurodegeneration with brain iron accumulation
383:
Neuroferritinopathy is most commonly diagnosed using
993:
421:-negative fibers are also often found in the muscle
205:, all physical symptoms of the body associated with
115:
and is caused by mutations in the gene encoding the
1063:
997:
48:
26:
21:
105:, and cognitive deficits which worsen with age.
479:. Parkinsonian symptoms were not decreased by
341:neurodegeneration with brain iron accumulation
8:
994:
941:Levi, Sonia; Finazzi, Dario (7 May 2014).
59:
35:
18:
968:
958:
818:
808:
797:Oxidative Medicine and Cellular Longevity
400:, causing neuronal death in these areas.
669:
266:that create oxidative molecules via the
93:of the human brain. Symptoms, which are
667:
665:
663:
661:
659:
657:
655:
653:
651:
649:
525:
483:. Iron supplements should be avoided.
77:characterized by the accumulation of
7:
748:International Review of Neurobiology
588:Parkinsonism & Related Disorders
298:The ferritin protein is made up of
899:10.1016/B978-0-7020-4087-0.00057-7
842:Rouault, Tracey A. (3 July 2013).
760:10.1016/B978-0-12-410502-7.00006-5
14:
889:Woimant, F; Trocello, JM (2014).
30:Adult-onset basal ganglia disease
600:10.1016/j.parkreldis.2012.06.021
1:
44:Cerebellum and basal ganglia
848:Nature Reviews Neuroscience
676:Nature Reviews Neuroscience
1116:
75:neurodegenerative disorder
947:Frontiers in Pharmacology
891:Disorders of heavy metals
514:Coenzyme Q10 (ubiquinone)
425:of affected individuals.
43:
34:
1043:C548080 C548080, C548080
960:10.3389/fphar.2014.00099
1100:Neurological disorders
496:
380:
632:"Neuroferritinopathy"
494:
404:Physiological testing
378:
419:cytochrome c oxidase
365:ferritin light chain
810:10.1155/2012/128647
325:Parkinson's disease
321:Alzheimer's disease
236:frameshift mutation
175:blood brain barrier
148:Diagnostic findings
71:Neuroferritinopathy
22:Neuroferritinopathy
1064:External resources
497:
381:
363:insertions in the
207:movement disorders
140:Signs and symptoms
1087:
1086:
185:Physical symptoms
158:neurodegeneration
108:This disorder is
68:
67:
16:Medical condition
1107:
995:
983:
982:
972:
962:
938:
921:
920:
886:
880:
879:
839:
833:
832:
822:
812:
788:
782:
781:
743:
708:
707:
671:
644:
643:
627:
612:
611:
583:
390:cerebral atrophy
295:→ Fe + HOO• + H
284:→ Fe + HO• + OH
273:Fenton Reaction
64:
63:
39:
19:
1115:
1114:
1110:
1109:
1108:
1106:
1105:
1104:
1090:
1089:
1088:
1083:
1082:
1059:
1058:
1006:
992:
987:
986:
940:
939:
924:
909:
888:
887:
883:
860:10.1038/nrn3453
841:
840:
836:
790:
789:
785:
770:
745:
744:
711:
688:10.1038/nrn1537
673:
672:
647:
629:
628:
615:
585:
584:
527:
522:
506:
489:
440:
431:
429:Genetic testing
406:
373:
337:
329:genetic testing
317:
304:light chain (L)
300:heavy chain (H)
294:
290:
283:
279:
268:Fenton Reaction
255:
222:
187:
150:
142:
119:subunit of the
58:
17:
12:
11:
5:
1113:
1111:
1103:
1102:
1092:
1091:
1085:
1084:
1081:
1080:
1068:
1067:
1065:
1061:
1060:
1057:
1056:
1045:
1034:
1023:
1007:
1002:
1001:
999:
998:Classification
991:
990:External links
988:
985:
984:
922:
907:
881:
854:(8): 551–564.
834:
783:
768:
709:
682:(11): 863–73.
645:
613:
524:
523:
521:
518:
505:
502:
495:Map of England
488:
485:
439:
436:
430:
427:
405:
402:
398:purkinje cells
372:
369:
336:
335:Classification
333:
316:
313:
292:
288:
281:
277:
254:
251:
221:
218:
186:
183:
149:
146:
141:
138:
134:founder effect
95:extrapyramidal
66:
65:
52:
46:
45:
41:
40:
32:
31:
28:
24:
23:
15:
13:
10:
9:
6:
4:
3:
2:
1112:
1101:
1098:
1097:
1095:
1079:
1075:
1074:
1070:
1069:
1066:
1062:
1055:
1051:
1050:
1046:
1044:
1040:
1039:
1035:
1033:
1029:
1028:
1024:
1022:
1018:
1017:
1013:
1009:
1008:
1005:
1000:
996:
989:
980:
976:
971:
966:
961:
956:
952:
948:
944:
937:
935:
933:
931:
929:
927:
923:
918:
914:
910:
908:9780702040870
904:
900:
896:
892:
885:
882:
877:
873:
869:
865:
861:
857:
853:
849:
845:
838:
835:
830:
826:
821:
816:
811:
806:
802:
798:
794:
787:
784:
779:
775:
771:
769:9780124105027
765:
761:
757:
753:
749:
742:
740:
738:
736:
734:
732:
730:
728:
726:
724:
722:
720:
718:
716:
714:
710:
705:
701:
697:
693:
689:
685:
681:
677:
670:
668:
666:
664:
662:
660:
658:
656:
654:
652:
650:
646:
641:
637:
633:
626:
624:
622:
620:
618:
614:
609:
605:
601:
597:
594:(8): 909–15.
593:
589:
582:
580:
578:
576:
574:
572:
570:
568:
566:
564:
562:
560:
558:
556:
554:
552:
550:
548:
546:
544:
542:
540:
538:
536:
534:
532:
530:
526:
519:
517:
515:
511:
503:
501:
493:
486:
484:
482:
478:
474:
470:
466:
462:
458:
454:
450:
449:Tetrabenazine
446:
437:
435:
428:
426:
424:
420:
416:
411:
403:
401:
399:
395:
391:
386:
377:
370:
368:
366:
362:
358:
354:
353:basal ganglia
350:
346:
342:
334:
332:
330:
326:
322:
314:
312:
308:
305:
301:
296:
285:
274:
271:
269:
265:
264:free radicals
260:
252:
250:
248:
247:free radicals
244:
239:
237:
232:
228:
219:
217:
214:
212:
208:
204:
200:
196:
192:
184:
182:
178:
176:
171:
167:
163:
159:
155:
147:
145:
139:
137:
135:
129:
127:
122:
118:
114:
111:
106:
104:
100:
96:
92:
88:
84:
83:basal ganglia
80:
76:
73:is a genetic
72:
62:
56:
53:
51:
47:
42:
38:
33:
29:
25:
20:
1071:
1047:
1036:
1025:
1010:
950:
946:
890:
884:
851:
847:
837:
800:
796:
786:
751:
747:
679:
675:
591:
587:
507:
498:
487:Epidemiology
457:orphenadrine
441:
432:
407:
382:
371:Neuroimaging
338:
318:
309:
297:
286:
275:
272:
257:The protein
256:
240:
223:
215:
211:parkinsonism
188:
179:
151:
143:
130:
107:
91:motor cortex
70:
69:
510:deferiprone
117:light chain
27:Other names
803:: 128647.
754:: 91–123.
520:References
473:clonazepam
415:aggregates
361:nucleotide
345:Nazi party
287:(2) Fe + H
276:(1) Fe + H
199:spasticity
154:cavitation
87:cerebellum
1054:699299001
1049:SNOMED CT
704:205500060
465:sulpiride
461:benzhexol
438:Treatment
315:Diagnosis
253:Mechanism
243:apoptosis
110:autosomal
55:Neurology
50:Specialty
1094:Category
1073:Orphanet
979:24847269
917:24365357
876:21302204
868:23820773
829:22701145
778:24209436
696:15496864
640:20301320
608:22818529
504:Research
469:diazepam
423:biopsies
259:ferritin
227:carboxyl
203:rigidity
195:dystonia
170:striatum
121:ferritin
113:dominant
103:dystonia
970:4019866
820:3369498
394:putamen
357:alleles
168:of the
162:neurons
81:in the
1078:157846
1032:606159
977:
967:
953:: 99.
915:
905:
874:
866:
827:
817:
776:
766:
702:
694:
638:
606:
512:, and
481:L-Dopa
477:deanol
475:, and
453:L-Dopa
220:Causes
201:, and
191:chorea
156:, and
99:chorea
89:, and
57:
1021:G23.0
872:S2CID
700:S2CID
445:Botox
410:serum
1038:MeSH
1027:OMIM
975:PMID
913:PMID
903:ISBN
864:PMID
825:PMID
801:2012
774:PMID
764:ISBN
692:PMID
636:PMID
604:PMID
302:and
231:exon
166:glia
164:and
79:iron
1012:ICD
965:PMC
955:doi
895:doi
856:doi
815:PMC
805:doi
756:doi
752:110
684:doi
596:doi
385:MRI
379:MRI
323:or
126:MRI
1096::
1076::
1052::
1041::
1030::
1019::
1016:10
973:.
963:.
949:.
945:.
925:^
911:.
901:.
870:.
862:.
852:14
850:.
846:.
823:.
813:.
799:.
795:.
772:.
762:.
750:.
712:^
698:.
690:.
678:.
648:^
634:.
616:^
602:.
592:18
590:.
528:^
516:.
471:,
467:,
463:,
459:,
455:,
331:.
238:.
197:,
193:,
101:,
85:,
1014:-
1004:D
981:.
957::
951:5
919:.
897::
878:.
858::
831:.
807::
780:.
758::
706:.
686::
680:5
642:.
610:.
598::
293:2
291:O
289:2
282:2
280:O
278:2
Text is available under the Creative Commons Attribution-ShareAlike License. Additional terms may apply.