199:
environment. The amount of pressure required to cause nerve dysfunction starts at around 20mmHg where epineural venus blood flow is reduced. At 30mmHg anterograde and retrograde axonal transport is impaired. Between 30-50mmHg there will usually be changes in intraneural blood flow, axonal transport, and vascular permeability simultaneously. And at 80mmHg all intraneural blood flow is arrested, which results in a complete metabolic block. The amount of pressure required to disrupt intraneural blood flow isn't an absolute pressure but rather a function of the arterial blood pressure and perfusion pressure. Patients with higher blood pressures are somewhat protected from the effects of nerve entrapment by requiring higher pressures to interrupt intraneural blood flow. If these same patients are treated successfully for their hypertension, they may develop symptoms if they already had some latent, subclinical form of nerve compression.
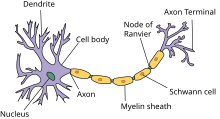
523:, and a very long axon that extends all the way to the innervation target. These nerves are as long as 1-1.5 meters (sciatic nerve). Most of the substances the axon needs to survive is manufactured in the cell body. The axon's survival depends on its connection with the cell body, supported by the axonal transport mechanisms to carry cellular material. The axonal transport system carries material along the axon in both directions (anterograde and retrograde) at different speeds (fast and slow). The fast transport travels at up to 400 mm/day. The slow transport is less than 8 mm/day. During compression not severe enough to cause axonmetesis (not destroy the axon), the axons will maintain their structural integrity but experience degraded function in the axonal transport systems. Studies have found that pressures as low as 30mmHg can impair axonal transport.
434:. These symptoms represent a conduction blockade where nerve signals can't be adequately transmitted along the length of the nerve. These symptoms are caused specifically by metabolic blocks, demyelination, and axonmetesis. A metabolic block is the temporary deprivation of nourishment from the blood supply which is readily reversed if the ischema does not last too long. Demyelination will interfere with conduction of signals along the nerve. Axonmetesis will result in a complete conduction block as Wallerian degeneration will destroy every part of the axon distal to the lesion if/until the axon regrows completely to its most distal innervation target.
462:. The symptoms represent hyperexcitability of a nerve where a signal is sent along a nerve due to a lower threshold for activation resulting in spontaneous signals. Demyelination can cause positive sensory symptoms such as pain due to increased ectopic firing. Demyelinated nerve tissue has been found to have a lower activation threshold for sending a signal, specifically for mechanosensitivity (e.g. light touch). While is some debate about the role of central nervous system sensitization in painful entrapment neuropathies, the success of peripheral nerve blocks suggests a peripheral nerve origin of this neuropathic pain.
17:
208:
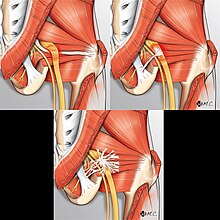
548:(like a seat belt) or creating a fibrous tunnel that is capable of pinching the nerve under pressure due to its toughness. In advanced cases, scar tissue can be found in all layers of the nerve impairing blood flow and essential functions of various tissue types. This is to say that scar tissue is fairly robust in its capability to injure nerves. It can do so through traction (fibrovascular attachments), compression (osteofibrous tunnels), or can be associated with an inflammatory response that injured tissue (fibrosis).
349:, epineural fibrosis and perineural thickening can be seen. This scarring is an irreversible change associated with nerve entrapment. If the scarring damages the microcirculatory environment, then the impaired blood supply will also be permanent. In cases where permanent impairment exists even after a nerve decompression, it's thought that the pathophysiological basis is due to extensive scarring along and within the nerve, as demyelination and axonmetesis are generally capable of healing but scarring cannot be reversed.
258:
interruptions in vascular supply. Both the acute and chronic forms of nerve entrapment involve initial changes in the microcirculatory environment. For the acute model, the sequence of events is typically an interruption of the blood supply followed by a metabolic block as the nerve stops functioning. For the chronic model, the sequence of events is a breakdown in the blood-nerve-barrier, followed by endoneurial edema and connective tissue fibrosis, followed by demyelination, and finally axonmetesis.
272:
injuries at the edge of the cuff, and this is called the "edge effect". The physical basis for the edge effect is believed to be a pressure gradient that deforms and then injures nerve tissue, and the pressure gradient is highest at the edges. At a microscopic level, intraneural blood vessels and nerve fibers are displaced longitudinally by shear strain. Surprisingly, smaller nerve fibers are more resistant to compression than large nerve fibers.
147:
410:
function and the hyperexcitability of nerve tissue. Additionally, nerve fibers may be differently affected by compression/ischema depending on their size, location and topography. Studies on human tissues have no found a clear correlation between the amount of structural damage to a nerve and the degree of symptoms. Patients can have significant symptoms without nerve fiber changes.
84:
112:, a tissue matrix analogous to the internal epineurium, and the nerve cells. The endoneurium has many small blood capillaries (endoneurial microvessels) which directly supply the nerves themselves. These capillaries have tight junctions to prevent the free flow of materials between cells and instead require substances to pass through the endothelial cells.
245:
immediate recovery. A single adhesion tethers the nerve in two directions - between the spinal root to the adhesion and between the adhesion to the terminal branches. These injuries will lead to edema and fibrosis, not just in the nerve but also the surrounding tissues touching the nerve, which may further inhibit normal nerve gliding in a vicious cycle.
486:. As nerve entrapment can leave individual nerves in different stages of injury, mixed lesions may be present. For example, mild/moderate entrapment may largely see an overlap of metabolic block and type I injury (local myelin sheath damage). Moderate/severe entrapment may see type I and II injuries simultaneously (myelin sheath damage and axon damage).
512:. Conceptually, this is analogous to multiple water filters in a filtration system (one for large particles, one for bacteria, etc). The water will be cleanest just past the last filter, but the filtration was due to the combined effects of the separate filters. To disable filtration, each of the filters must be removed rather than the last filter.
76:, which are short and concentrically wrapped around the diameter of an axon to give the appearance of a sausage-like mass and called a myelin sheath. The schwann cells are arranged in pattern such all parts of the axon are wrapped in schwann cells and successive schwann cells are separated by a very small distance. This separation gap is called a
49:
361:. This only affects the myelin sheath on myelinated axon while the axon and nerve continuity will remain preserved. Loss of myelin is often readily seen in histological samples as the layer of myelin around myelinated nerves will appear very thin, representing either the late stages of demyelination or early stages of remyelination.
68:. The cell body resides in the spinal cord and the axon extends all the way to the innervation target of the nerve. Peripheral nerve axons can be longer than 100 cm as they may need to travel along the full length of a limb to reach their innervation target, while the cell body is only 100 micrometers long. Nerves may be
344:
Lymphocytes, fibroblasts, and macrophages will also be able to cross the newly permeable blood nerve barrier and react to the antigens contained in the perineural space triggering an inflammatory reaction. As part of this inflammatory reaction, there will be excess deposits of fibrin (i.e. scarring).
271:
Direct pressure can physically deform the structure of the nerve. Local pressure can create a bidirectional displacement of nerve tissue from away from the area of compression by squishing the compressed tissue outwards. Studies using a cuff to compress a nerve have found the earliest and most severe
154:
Pressure can interrupt or arrest the microcirculatory environment of the nerve starting a pathophysiological cascade. As the heart beats, it pushes blood through arteries/arterioles/capillaries. Blood also travels through veins though more passively via valves and the assistance of muscles to squeeze
503:
due to injury at another site. This is due to impairment of the anterograde axonal transport mechanism, and with multiple lesions impairing anterograde axonal transport, the anterograde transport system will be most impacted just distal to the most distal entrapment. The basis of this theory was the
292:
The first sign of impairment to intraneural blood flow occurs in the epineural blood vessels at about 20-30mm Hg pressure. At pressures of 60-80mmHg there will be complete ischemia. A metabolic block can also be induced by stretching. In animal studies, venous statis was seen at an 8% stretch and at
211:
Fibrovascular bands are dense bands of scar tissue with a vascular supply that can restrict mobility of the sciatic nerve. Top left is a compressive / bridge-type band, like a seat belt. Top right is an adhesive / horse-strap band, like a leash. Bottom center is undefined distribution that restricts
162:
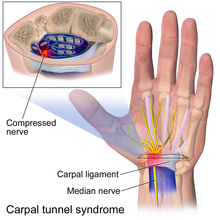
Compression is especially likely in anatomic tunnels or fibro-osseous spaces where there may be a conflict with the amount of free space available and the volume of the contents. If the tunnel narrows or if the contents of the tunnel expand, there will be an increase in pressure. Examples of tunnels
158:
For compression to affect nerve function, pressure needs to be applied non-uniformly. For example, frogs can survive in isolated pressure chambers at high pressures but much lower local compression can block conduction of the nerve. Scuba divers can dive to tens of meters of water depth and will not
27:
involves a cascade of physiological changes caused by compression and tension. Some of these changes are irreversible. The magnitude and duration of the forces determines the extent of injury. In the acute form, mechanical injury and metabolic blocks impede nerve function. In the chronic form, there
409:
Nerve entrapment is a complex lesion involving the multiple tissue types in a fascicle. There may be mixed lesions where individual tissue lesions contribute to the whole of the symptoms. Tissue injury may contribute to positive and/or negative symptoms, which can be attributed to the loss of nerve
322:
Intraneural blood vessels, similar to other microvessels in the human body, increase their permeability in response to stress. During extended periods of metabolic stress, such as ischema caused by compression, the blood-nerve-barrier will increase in permeability. This increase in the permeability
280:
Nerve function depends on its blood supply. Arresting or inhibiting the blood supply can deprive nerve tissue of oxygen and other essential nutrients to induce a metabolic block, whereby the nerve is unable to function. This block is purely a physiologic problem such that the structure of the nerve
248:
The most commonly understood mechanism of impaired nerve gliding is through the formation of scar tissue that adheres separate tissue planes. It is not always clear how the initial scar tissue forms, but once formed there is a clear path for the formation of further scar tissue - movement can cause
236:
at the elbow. The median nerve moves 9.6mm with wrist flexion and extension. This nerve movement also applies to the spinal nerves, which can stretch and slacken with movement of the spine. This nerve gliding happens at intraneurial and extraneurial tissue planes. Outside the nerve, a thin layer of
526:
The double-crush theory originally referred to anterograde axonal transport. For example, a spinal compressive lesion was posited to increase susceptibility to more distal compressive lesions like carpal tunnel. There is a complimentary reverse double-crush theory which refers to retrograde axonal
198:
Studies on compression and nerve function have found a dose-respondent relationship between pressure and duration. That is higher pressures and longer duration are associated with greater dysfunction. However even short but repeated periods of compression can also damage a nerve's microcirculatory
547:
in the deep gluteal space), it's the most common cause. While the concept of scar tissue causing traction injuries is widely accepted, its role is more complex than strictly causing stretching injuries. Scar tissue itself is very dense and is capable of applying pressure on a nerve through bands
257:
The pathophysiology of entrapment is complex because nerve tissue has many components (e.g. axon, myelin, endoneurium, perineurium, epineurium, blood vessels, etc) that may respond differently to various stressors affecting nerve function. The underlying mechanism of injury typically starts with
137:
Nerve entrapment is caused primarily by two physical forces on soft tissue: compression and tension. Compression will squeeze the nerve and impair its local microcirculatory environment which commonly happens in anatomic tunnels. Tension is a pulling force, often caused by scarring which impedes
120:
The peripheral blood nerve barrier is analogous to the blood brain barrier. Like the blood brain barrier, the blood nerve barrier creates a stable, privileged environment where certain substances cannot pass through due to tight junctions. The blood nerve barrier is made up of inner cells of the
364:
The pathology of fascicle to fascicle can vary. For example in some studies the central fascicles have appeared normal, while the peripheral fascicles showed significant thinning of myelin. Even within a fascicle, demyelination does not affect nerves uniformly. For example, in the early stages,
494:
Double crush syndrome is a theory of nerve injury first proposed by Upton and Thomas in 1972. The double crush theory is considered to be somewhat controversial, as there are disagreements over its existence and the underlying mechanisms that could produce it. It posits that neural function is
244:
Inhibition of normal gliding at these tissue planes can lead to repetitive stretch injuries during movements. Studies on rabbit sciatic nerves have found that even a 6% acute stretch can lead to significant impairment with recovery and a 12% acute stretch can lead to complete impairment and no
331:
As the blood-nerve-barrier breaks down, proteins and cells will be able to enter the perineural and endoneurial space. The increased permeability allowing substances to enter combined with the lack of a lymphatic system to drain fluids causes an increase in pressure and may alter the ionic
281:
is unchanged. If the metabolic block is short in duration, it is completely reversible with no permanent effects. An example of a metabolic block is when a limb "falls asleep" (temporary numbness, paresthesia, and weakness) due to the position of a limb that restricts blood flow. Complete
388:
where the endoneurial tubes are preserved. If an axon is injured, the axonal transport system may not function. Since the axon depends on its connection to the cell body, the disrupted axonal transport will cause segmental death of the axon distal to the injury site in a process called
309:
Like acute compression, chronic compression starts with the impairment of the microcirculatory environment. Studies on pressure have identified a "critical pressure level", above which the nerve is significantly impaired. This pressure level is 30mmHg below diastolic or 45mmHg below
249:
stretch injuries at the soft tissue attachments of the adhesion, triggering edema and further fibrosis of the nerve bed and potentially extending within the nerve itself. In deep gluteal syndrome, scar issue is the most common cause of sciatic nerve entrapment.
104:. The internal epineurium acts as soft cushion for the fascicles. A nerve fiber may have a variable number of fascicles, but there will be at least one (otherwise there would be no nerve cells). Fascicles are surrounded by a tissue layer called the
401:(sensory nerve). Provided that the endoneurial tube is not disrupted, there is still a pathway for the axon at the injury site to regrow, but the growth is very slow (approximately 1mm/day). Recovery can take months and is often partial.
300:
see an immediate improvement in their symptoms, and this is thought to be the restoration of blood flow after a metabolic block as other forms of functional nerve impairment such as neuropraxia and axonmetesis take longer to recover.
289:, is followed by hyperexcitability and then loss of nerve function over 60-90 minutes. The ischema is immediately reversible when the block is released, as long as the duration of ischema is not too long, such as 1-2 hours.
340:
is triggered, the swelling will last many hours the point that the entrapment is relieved. For example, following 2-8 hours of compression, endoneurial fluid pressure will rapidly rise and can stay elevated for 24 hours.
159:
experience any form of nerve compression, but the same pressure divers experience under 1 meter of water (pressure under 1m of water is 10k Pascal ~ 80mmHg) applied locally can completely arrest nerve function.
175:. Sometimes compression occurs in areas that are not considered tunnels and where a nerve passes between two mechanically stiffer tissue types that can squeeze or pinch the soft nerve. Examples include the
96:
The axons of nerve cells are surrounded by various connective tissue layers and bundled together in a structure called a nerve fiber. At the surface of a nerve fiber is a tissue layer called the
1431:
Howe JF, Loeser JD, Calvin WH (February 1977). "Mechanosensitivity of dorsal root ganglia and chronically injured axons: a physiological basis for the radicular pain of nerve root compression".
1689:
Hernando MF, Cerezal L, Pérez-Carro L, Abascal F, Canga A (July 2015). "Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space".
150:
Carpal tunnel syndrome is caused by compression of the median nerve at the carpal tunnel. The carpal tunnel is formed by the bones of the wrist and the transverse carpal ligament.
1567:
Schmid AB, Coppieters MW (December 2011). "The double crush syndrome revisited--a Delphi study to reveal current expert views on mechanisms underlying dual nerve disorders".
365:
demyelination can be seen at the edge of fascicles near the periphery of the nerve, and in later stages the demyelination is diffusely seen within the entirety of a fasicle.
1421:
Chaney B, Nadi M. Axonotmesis. . In: StatPearls . Treasure Island (FL): StatPearls
Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562304/
1239:
Szabo RM, Gelberman RH, Williamson RV, Hargens AR (1983). "Effects of increased systemic blood pressure on the tissue fluid pressure threshold of peripheral nerve".
20:
Histological comparison of a normal nerve and an atrophied nerve using a cross-slice of the sciatic nerve. Left is a normal nerve. Right is an atrophied nerve.
1735:
976:
Wall EJ, Massie JB, Kwan MK, Rydevik BL, Myers RR, Garfin SR (January 1992). "Experimental stretch neuropathy. Changes in nerve conduction under tension".
80:. Unmyelinated nerves are also surrounded by schwann cells but the schwann cells are not wrapped around the axon multiple times to form a myelin sheath.
36:, and finally followed by axonmetesis. The injury will often be a mixed lesion where mild/moderate compression is a combination of a metabolic block and
384:
For severe nerve entrapment, nerve axons can be injured to the point of destruction. Axon injury is also known as axonmetesis or a
Sunderland type 2
1468:"John J. Bonica Award Lecture: Peripheral neuronal hyperexcitability: the "low-hanging" target for safe therapeutic strategies in neuropathic pain"
1011:
Rydevik B, Lundborg G, Bagge U (January 1981). "Effects of graded compression on intraneural blood blow. An in vivo study on rabbit tibial nerve".
357:
By the time chronic nerve compression becomes symptomatic, myelin tissue in the area of compression is likely damaged triggering a process called
376:. It can cause a local conduction block for weeks to months as the myelin sheaths regrow, assuming no reinjury which would prolong recovery.
1352:
Mackinnon SE, Dellon AL, Hudson AR, Hunter DA (March 1986). "Histopathology of compression of the superficial radial nerve in the forearm".
1387:
O'Brien JP, Mackinnon SE, MacLean AR, Hudson AR, Dellon AL, Hunter DA (November 1987). "A model of chronic nerve compression in the rat".
618:"Etiology, Diagnosis, and Treatment of Dynamic Nerve Compression Syndromes of the Elbow Among High-Level Pitchers: A Review of 7 Cases"
314:. Interestingly, patients with higher blood pressure require larger compressive forces to interrupt the microcirculatory environment.
176:
100:
or sometimes external epineurium. Within the epineurium there is a connective tissue matrix called the internal epineurium and
1274:
Mackinnon SE, Dellon AL, Hudson AR, Hunter DA (August 1984). "Chronic nerve compression--an experimental model in the rat".
188:
138:
nerve mobility during limb movements. Both the magnitude and duration of these forces can determine the extent of injury.
241:
surrounds the nerve upon which the epineurial surface glides. Inside the nerve, fascicles can glide against each other.
722:
Lundborg G, Dahlin LB (May 1996). "Anatomy, function, and pathophysiology of peripheral nerves and nerve compression".
16:
572:
483:
385:
373:
207:
191:. The compression even be dynamic, where compression may only be present during certain activities and positions. In
1314:
Mackinnon SE, Dellon AL, Hudson AR, Hunter DA (1986). "Chronic human nerve compression--a histological assessment".
562:
233:
221:
24:
1730:
938:
Dahlin LB (January 1991). "Aspects on pathophysiology of nerve entrapments and nerve compression injuries".
311:
577:
509:
390:
587:
567:
540:
500:
192:
184:
33:
874:
Rydevik B, Brown MD, Lundborg G (1984). "Pathoanatomy and pathophysiology of nerve root compression".
333:
582:
297:
323:
in the blood-nerve-barrier is the first pathological symptom observed during compression studies.
1706:
1671:
1622:
1584:
1546:
1497:
1448:
1404:
1369:
1331:
1291:
1256:
1221:
1167:
1118:
1069:
1028:
993:
955:
891:
803:
739:
647:
180:
155:
veins. If there is localized pressure high enough, it can interrupt the normal flow of blood.
1698:
1661:
1653:
1614:
1576:
1536:
1528:
1487:
1479:
1440:
1396:
1361:
1323:
1283:
1248:
1211:
1201:
1157:
1149:
1108:
1100:
1059:
1020:
985:
947:
883:
795:
731:
637:
629:
126:
28:
is a sequence of changes starting with a breakdown of the blood-nerve-barrier, followed by
419:
394:
217:
77:
216:
Peripheral nerves frequently glide during movement of the extremities. For example, the
1666:
1641:
1541:
1516:
1492:
1467:
1327:
1216:
1189:
1162:
1137:
1113:
1088:
1064:
1047:
642:
617:
516:
172:
146:
101:
1618:
1605:
Upton AR, McComas AJ (August 1973). "The double crush in nerve entrapment syndromes".
1365:
1024:
951:
799:
735:
1724:
1444:
1400:
1287:
887:
544:
505:
459:
358:
168:
164:
1483:
83:
989:
470:
As the majority of nerve entrapment doesn't affect the structural integrity of the
447:
431:
427:
398:
73:
1657:
482:, the nerve injuries from nerve entrapment will primarily be type I or II in the
108:
which is a protective sheath that acts as a barrier. Inside the fascicles is the
520:
475:
471:
443:
369:
122:
109:
105:
37:
1580:
1532:
1702:
1190:"Endoscopic Sciatic Neurolysis for Deep Gluteal Syndrome: A Systematic Review"
479:
286:
238:
97:
633:
40:, while severe compression combines elements of neuropraxia and axonmetesis.
1104:
368:
Damage to the myelin sheath of nerves is a nerve injury. It's classified as
346:
225:
1710:
1675:
1588:
1550:
1501:
1252:
1225:
1171:
1122:
1073:
807:
651:
228:
of the shoulder. The median/ulnar nerves move 7.3mm and 9.8mm during elbow
195:, patients often have sciatic radiculopathy when sitting but not standing.
1626:
1408:
1373:
1335:
1295:
1260:
1153:
1089:"Superior and Middle Cluneal Nerve Entrapment as a Cause of Low Back Pain"
1032:
997:
959:
895:
743:
336:" leading to post-traumatic ischemia of the nerve cells. When endoneurial
1452:
1206:
332:
environment. The increased pressure in the endoneurium can cause a mini "
282:
1642:"Axonal transport: cargo-specific mechanisms of motility and regulation"
72:
or unmyelinated. Myelinated nerves have the axon covered by segments of
423:
229:
69:
61:
1640:
Maday S, Twelvetrees AE, Moughamian AJ, Holzbaur EL (October 2014).
557:
455:
337:
206:
145:
82:
48:
47:
29:
15:
786:
Mackinnon SE (May 2002). "Pathophysiology of nerve compression".
499:, having been compressed at one site, are susceptible to further
536:
496:
451:
65:
393:. This will result in a complete conduction block, leading to
64:
comprise a small cell body and a very long segment called the
212:
mobility in multiple directions, like a splattering of glue.
1466:
Raja SN, Ringkamp M, Guan Y, Campbell JN (September 2020).
442:
Positive symptoms are those for which function is gained:
539:
formation is a major cause of nerve entrapment, and for
418:
Negative symptoms are those for which function is lost:
293:
a 15% stretch the blood supply was completely arrested.
296:
It's a frequent occurrence that patients receiving a
515:
The structure of peripheral nerves includes a small
32:
with connective tissue changes, followed by diffuse
1048:"Meralgia paresthetica: a review of the literature"
1046:Cheatham SW, Kolber MJ, Salamh PA (December 2013).
1087:Isu T, Kim K, Morimoto D, Iwamoto N (March 2018).
1136:Martin HD, Reddy M, Gómez-Hoyos J (July 2015).
8:
616:von Bergen TN, Lourie GM (November 2018).
1665:
1540:
1491:
1215:
1205:
1161:
1112:
1063:
641:
599:
1347:
1345:
1183:
1181:
133:Physical forces which cause entrapment
1600:
1598:
1562:
1560:
1309:
1307:
1305:
933:
931:
929:
927:
925:
869:
867:
865:
863:
861:
859:
857:
855:
853:
851:
849:
847:
845:
843:
841:
839:
837:
781:
779:
777:
775:
773:
717:
715:
713:
711:
709:
707:
705:
703:
701:
699:
697:
695:
693:
691:
689:
687:
685:
683:
681:
7:
1515:Molinari WJ, Elfar JC (April 2013).
971:
969:
923:
921:
919:
917:
915:
913:
911:
909:
907:
905:
835:
833:
831:
829:
827:
825:
823:
821:
819:
817:
771:
769:
767:
765:
763:
761:
759:
757:
755:
753:
679:
677:
675:
673:
671:
669:
667:
665:
663:
661:
611:
609:
607:
605:
603:
1736:Peripheral nervous system disorders
1188:Metikala S, Sharma V (March 2022).
372:or a type 1 nerve injury using the
327:Edema and connective tissue changes
1328:10.1111/j.1365-2990.1986.tb00159.x
189:long posterior sacroiliac ligament
52:Anatomy of a myelinated nerve cell
14:
1401:10.1097/00000637-198711000-00008
1288:10.1097/00000637-198408000-00004
888:10.1097/00007632-198401000-00004
318:Breakdown of blood-nerve barrier
1484:10.1097/j.pain.0000000000001838
285:, such as the application of a
177:lateral femoral cutaneous nerve
990:10.1302/0301-620X.74B1.1732240
1:
1619:10.1016/s0140-6736(73)93196-6
1366:10.1016/s0363-5023(86)80052-1
1025:10.1016/s0363-5023(81)80003-2
952:10.1016/S1042-3680(18)30754-X
800:10.1016/s0749-0712(01)00012-9
736:10.1016/S0749-0712(21)00303-6
432:diminished or absent reflexes
1658:10.1016/j.neuron.2014.10.019
1445:10.1016/0304-3959(77)90033-1
1517:"The double crush syndrome"
573:Nerve injury classification
1752:
1581:10.1016/j.math.2011.05.005
1533:10.1016/j.jhsa.2012.12.038
1316:Neuropathol Appl Neurobiol
563:Nerve compression syndrome
1703:10.1007/s00256-015-2124-6
484:Sunderland classification
374:Sunderland classification
220:can move up to 50mm with
1527:(4): 799–801, quiz 801.
634:10.1177/2325967118807131
628:(11): 2325967118807131.
495:impaired because single
87:Anatomy of a nerve fiber
44:Peripheral nerve anatomy
1138:"Deep gluteal syndrome"
1105:10.14245/ns.1836024.012
312:systolic blood pressure
1253:10.1002/jor.1100010208
1052:Int J Sports Phys Ther
578:Carpal tunnel syndrome
510:carpal tunnel syndrome
508:seen in patients with
504:high rate of cervical
466:Degree of nerve injury
391:Wallerian degeneration
213:
151:
88:
53:
21:
876:Spine (Phila Pa 1976)
588:Deep gluteal syndrome
541:deep gluteal syndrome
490:Double crush syndrome
448:increased sensitivity
347:histological analysis
210:
193:deep gluteal syndrome
185:middle cluneal nerves
149:
86:
51:
19:
1478:(Suppl 1): S14–S26.
1207:10.7759/cureus.23153
978:J Bone Joint Surg Br
405:Clinical correlation
334:compartment syndrome
121:perineurium and the
1154:10.1093/jhps/hnv029
940:Neurosurg Clin N Am
622:Orthop J Sports Med
583:Piriformis syndrome
543:(entrapment of the
531:Role of scar tissue
305:Chronic compression
298:nerve decompression
125:of the endoneurial
116:Blood nerve barrier
1142:J Hip Preserv Surg
237:tissue similar to
214:
152:
89:
54:
22:
438:Positive symptoms
414:Negative symptoms
397:(motor nerve) or
267:Mechanical injury
262:Acute compression
181:inguinal ligament
123:endothelial cells
1743:
1715:
1714:
1686:
1680:
1679:
1669:
1637:
1631:
1630:
1613:(7825): 359–62.
1602:
1593:
1592:
1564:
1555:
1554:
1544:
1512:
1506:
1505:
1495:
1463:
1457:
1456:
1428:
1422:
1419:
1413:
1412:
1384:
1378:
1377:
1349:
1340:
1339:
1311:
1300:
1299:
1271:
1265:
1264:
1236:
1230:
1229:
1219:
1209:
1185:
1176:
1175:
1165:
1133:
1127:
1126:
1116:
1084:
1078:
1077:
1067:
1043:
1037:
1036:
1008:
1002:
1001:
973:
964:
963:
935:
900:
899:
871:
812:
811:
783:
748:
747:
719:
656:
655:
645:
613:
25:Nerve entrapment
1751:
1750:
1746:
1745:
1744:
1742:
1741:
1740:
1731:Pathophysiology
1721:
1720:
1719:
1718:
1691:Skeletal Radiol
1688:
1687:
1683:
1639:
1638:
1634:
1604:
1603:
1596:
1566:
1565:
1558:
1514:
1513:
1509:
1465:
1464:
1460:
1430:
1429:
1425:
1420:
1416:
1386:
1385:
1381:
1351:
1350:
1343:
1313:
1312:
1303:
1273:
1272:
1268:
1238:
1237:
1233:
1187:
1186:
1179:
1135:
1134:
1130:
1086:
1085:
1081:
1045:
1044:
1040:
1010:
1009:
1005:
975:
974:
967:
937:
936:
903:
873:
872:
815:
785:
784:
751:
721:
720:
659:
615:
614:
601:
596:
554:
533:
492:
468:
440:
420:muscle weakness
416:
407:
395:muscle weakness
382:
355:
329:
320:
307:
278:
276:Metabolic block
269:
264:
255:
218:brachial plexus
205:
144:
135:
118:
94:
78:node of Ranvier
59:
46:
12:
11:
5:
1749:
1747:
1739:
1738:
1733:
1723:
1722:
1717:
1716:
1681:
1652:(2): 292–309.
1632:
1594:
1556:
1521:J Hand Surg Am
1507:
1458:
1423:
1414:
1389:Ann Plast Surg
1379:
1354:J Hand Surg Am
1341:
1301:
1276:Ann Plast Surg
1266:
1231:
1177:
1128:
1079:
1038:
1013:J Hand Surg Am
1003:
965:
901:
813:
749:
657:
598:
597:
595:
592:
591:
590:
585:
580:
575:
570:
565:
560:
553:
550:
532:
529:
491:
488:
467:
464:
460:fasciculations
439:
436:
415:
412:
406:
403:
381:
378:
354:
351:
328:
325:
319:
316:
306:
303:
277:
274:
268:
265:
263:
260:
254:
251:
204:
201:
173:cubital tunnel
143:
140:
134:
131:
117:
114:
93:
90:
58:
55:
45:
42:
13:
10:
9:
6:
4:
3:
2:
1748:
1737:
1734:
1732:
1729:
1728:
1726:
1712:
1708:
1704:
1700:
1697:(7): 919–34.
1696:
1692:
1685:
1682:
1677:
1673:
1668:
1663:
1659:
1655:
1651:
1647:
1643:
1636:
1633:
1628:
1624:
1620:
1616:
1612:
1608:
1601:
1599:
1595:
1590:
1586:
1582:
1578:
1575:(6): 557–62.
1574:
1570:
1563:
1561:
1557:
1552:
1548:
1543:
1538:
1534:
1530:
1526:
1522:
1518:
1511:
1508:
1503:
1499:
1494:
1489:
1485:
1481:
1477:
1473:
1469:
1462:
1459:
1454:
1450:
1446:
1442:
1438:
1434:
1427:
1424:
1418:
1415:
1410:
1406:
1402:
1398:
1394:
1390:
1383:
1380:
1375:
1371:
1367:
1363:
1360:(2): 206–10.
1359:
1355:
1348:
1346:
1342:
1337:
1333:
1329:
1325:
1322:(6): 547–65.
1321:
1317:
1310:
1308:
1306:
1302:
1297:
1293:
1289:
1285:
1282:(2): 112–20.
1281:
1277:
1270:
1267:
1262:
1258:
1254:
1250:
1246:
1242:
1235:
1232:
1227:
1223:
1218:
1213:
1208:
1203:
1200:(3): e23153.
1199:
1195:
1191:
1184:
1182:
1178:
1173:
1169:
1164:
1159:
1155:
1151:
1148:(2): 99–107.
1147:
1143:
1139:
1132:
1129:
1124:
1120:
1115:
1110:
1106:
1102:
1098:
1094:
1090:
1083:
1080:
1075:
1071:
1066:
1061:
1058:(6): 883–93.
1057:
1053:
1049:
1042:
1039:
1034:
1030:
1026:
1022:
1018:
1014:
1007:
1004:
999:
995:
991:
987:
983:
979:
972:
970:
966:
961:
957:
953:
949:
945:
941:
934:
932:
930:
928:
926:
924:
922:
920:
918:
916:
914:
912:
910:
908:
906:
902:
897:
893:
889:
885:
881:
877:
870:
868:
866:
864:
862:
860:
858:
856:
854:
852:
850:
848:
846:
844:
842:
840:
838:
836:
834:
832:
830:
828:
826:
824:
822:
820:
818:
814:
809:
805:
801:
797:
794:(2): 231–41.
793:
789:
782:
780:
778:
776:
774:
772:
770:
768:
766:
764:
762:
760:
758:
756:
754:
750:
745:
741:
737:
733:
730:(2): 185–93.
729:
725:
718:
716:
714:
712:
710:
708:
706:
704:
702:
700:
698:
696:
694:
692:
690:
688:
686:
684:
682:
680:
678:
676:
674:
672:
670:
668:
666:
664:
662:
658:
653:
649:
644:
639:
635:
631:
627:
623:
619:
612:
610:
608:
606:
604:
600:
593:
589:
586:
584:
581:
579:
576:
574:
571:
569:
568:Demyelination
566:
564:
561:
559:
556:
555:
551:
549:
546:
545:sciatic nerve
542:
538:
530:
528:
524:
522:
518:
513:
511:
507:
506:radiculopathy
502:
498:
489:
487:
485:
481:
477:
473:
465:
463:
461:
457:
456:muscle spasms
453:
449:
445:
437:
435:
433:
429:
425:
421:
413:
411:
404:
402:
400:
396:
392:
387:
379:
377:
375:
371:
366:
362:
360:
359:demyelination
353:Demyelination
352:
350:
348:
342:
339:
335:
326:
324:
317:
315:
313:
304:
302:
299:
294:
290:
288:
284:
275:
273:
266:
261:
259:
252:
250:
246:
242:
240:
235:
231:
227:
223:
219:
209:
202:
200:
196:
194:
190:
186:
182:
178:
174:
170:
169:tarsal tunnel
166:
165:carpal tunnel
160:
156:
148:
141:
139:
132:
130:
128:
124:
115:
113:
111:
107:
103:
99:
91:
85:
81:
79:
75:
74:schwann cells
71:
67:
63:
56:
50:
43:
41:
39:
35:
34:demyelination
31:
26:
18:
1694:
1690:
1684:
1649:
1645:
1635:
1610:
1606:
1572:
1568:
1524:
1520:
1510:
1475:
1471:
1461:
1439:(1): 25–41.
1436:
1432:
1426:
1417:
1395:(5): 430–5.
1392:
1388:
1382:
1357:
1353:
1319:
1315:
1279:
1275:
1269:
1247:(2): 172–8.
1244:
1241:J Orthop Res
1240:
1234:
1197:
1193:
1145:
1141:
1131:
1099:(1): 25–32.
1096:
1092:
1082:
1055:
1051:
1041:
1016:
1012:
1006:
984:(1): 126–9.
981:
977:
943:
939:
879:
875:
791:
787:
727:
723:
625:
621:
534:
525:
514:
493:
469:
444:paresthesias
441:
417:
408:
386:nerve injury
383:
367:
363:
356:
343:
330:
321:
308:
295:
291:
279:
270:
256:
253:Pathogenesis
247:
243:
215:
197:
161:
157:
153:
136:
127:microvessels
119:
95:
60:
23:
1019:(1): 3–12.
946:(1): 21–9.
882:(1): 7–15.
537:scar tissue
527:transport.
521:spinal cord
476:perineurium
472:endoneurium
380:Axon injury
370:neuropraxia
142:Compression
110:endoneurium
106:perineurium
92:Nerve fiber
62:Nerve cells
38:neuropraxia
1725:Categories
1093:Neurospine
594:References
535:Extensive
501:neuropathy
480:epineurium
287:tourniquet
239:adventitia
98:epineurium
70:myelinated
57:Nerve cell
788:Hand Clin
724:Hand Clin
517:cell body
234:extension
226:adduction
222:abduction
102:fascicles
1711:25739706
1676:25374356
1589:21646036
1569:Man Ther
1551:23466128
1502:33090736
1226:35444897
1172:27011826
1123:29656623
1074:24377074
808:12371026
652:30480016
552:See also
428:numbness
399:numbness
183:and the
163:are the
1667:4269290
1627:4124532
1542:5823245
1493:7586453
1409:3688790
1374:3958448
1336:3561691
1296:6476732
1261:6679859
1217:9010003
1163:4718497
1114:5944640
1065:3867081
1033:7204915
998:1732240
960:1668263
896:6372124
744:8724572
643:6247494
519:at the
424:atrophy
283:ischema
230:flexion
203:Tension
187:at the
179:at the
1709:
1674:
1664:
1646:Neuron
1625:
1607:Lancet
1587:
1549:
1539:
1500:
1490:
1453:195255
1451:
1407:
1372:
1334:
1294:
1259:
1224:
1214:
1194:Cureus
1170:
1160:
1121:
1111:
1072:
1062:
1031:
996:
958:
894:
806:
742:
650:
640:
171:, and
558:Nerve
497:axons
478:, or
338:edema
30:edema
1707:PMID
1672:PMID
1623:PMID
1585:PMID
1547:PMID
1498:PMID
1472:Pain
1449:PMID
1433:Pain
1405:PMID
1370:PMID
1332:PMID
1292:PMID
1257:PMID
1222:PMID
1168:PMID
1119:PMID
1070:PMID
1029:PMID
994:PMID
956:PMID
892:PMID
804:PMID
740:PMID
648:PMID
452:pain
232:and
224:and
66:axon
1699:doi
1662:PMC
1654:doi
1615:doi
1577:doi
1537:PMC
1529:doi
1488:PMC
1480:doi
1476:161
1441:doi
1397:doi
1362:doi
1324:doi
1284:doi
1249:doi
1212:PMC
1202:doi
1158:PMC
1150:doi
1109:PMC
1101:doi
1060:PMC
1021:doi
986:doi
948:doi
884:doi
796:doi
732:doi
638:PMC
630:doi
345:On
1727::
1705:.
1695:44
1693:.
1670:.
1660:.
1650:84
1648:.
1644:.
1621:.
1609:.
1597:^
1583:.
1573:16
1571:.
1559:^
1545:.
1535:.
1525:38
1523:.
1519:.
1496:.
1486:.
1474:.
1470:.
1447:.
1435:.
1403:.
1393:19
1391:.
1368:.
1358:11
1356:.
1344:^
1330:.
1320:12
1318:.
1304:^
1290:.
1280:13
1278:.
1255:.
1243:.
1220:.
1210:.
1198:14
1196:.
1192:.
1180:^
1166:.
1156:.
1144:.
1140:.
1117:.
1107:.
1097:15
1095:.
1091:.
1068:.
1054:.
1050:.
1027:.
1015:.
992:.
982:74
980:.
968:^
954:.
942:.
904:^
890:.
878:.
816:^
802:.
792:18
790:.
752:^
738:.
728:12
726:.
660:^
646:.
636:.
624:.
620:.
602:^
474:,
458:,
454:,
450:,
446:,
430:,
426:,
422:,
167:,
129:.
1713:.
1701::
1678:.
1656::
1629:.
1617::
1611:2
1591:.
1579::
1553:.
1531::
1504:.
1482::
1455:.
1443::
1437:3
1411:.
1399::
1376:.
1364::
1338:.
1326::
1298:.
1286::
1263:.
1251::
1245:1
1228:.
1204::
1174:.
1152::
1146:2
1125:.
1103::
1076:.
1056:8
1035:.
1023::
1017:6
1000:.
988::
962:.
950::
944:2
898:.
886::
880:9
810:.
798::
746:.
734::
654:.
632::
626:6
Text is available under the Creative Commons Attribution-ShareAlike License. Additional terms may apply.