169:
17:
217:
continuously disrupted abutment attachment surface and in reaction to this, bone loss occurred on the implant in order to provide the dimension necessary for the epithelium and soft connective tissue attachment to the implant fixture itself—this defined early implant placement and was often colloquially referred to as "bone loss to the first thread." This vertical loss of bone (
80:, during which time the surrounding bone grows into intimate contact with the surface of the implants and the implants become fused to the bone. When this process has been deemed to have occurred to a sufficient extent, the implants are fitted with restorative abutments in order to allow dental restorations (e.g.
335:
Furthermore, by platform switching implants that are 3 mm apart or less or within 1.5 mm of the facial aspect of a thin buccal plate, the implant-abutment junction (IAJ) is shifted onto the implant platform away from the peri-implant bone, mitigating the deleterious impact of the inflammatory zone at
147:
infiltrate that forms a zone around the IAJ. Although not yet fully understood, the current theory of the benefit of platform switching is related to the physical repositioning of the IAJ away from the outer edge of the implant and the surrounding bone, thereby containing the inflammatory infiltrate
67:
Discovered by accident in the late 1980s, the benefits of platform switching have become the focus of implant-related research with increasing frequency. Numerous peer-reviewed articles and recent systematic reviews have revealed that platform switching can be considered a means of preventing initial
282:
Because of this established mean horizontal dimension of the immediate crestal bone loss around dental implants, an issue arises when implants are placed into adjacent sites in the mouth. If the implants are placed too closely together, the overlap of the horizontal components of each implant's
216:
aspect of the implants because the abutment that attaches to the implant was often removed many times to allow for impression taking, abutment changing and other related clinical functions. As such, the epithelial and connective tissue protection for the bone was unable to reliably form on the
135:
It has been observed that some degree of bone resorption occurs at the crest of bone following implant placement. Through extensive investigation, it has been discovered that the extent of bone resorption is related to both the texture of the surfaces of the implant and abutment at and the
326:
and soft connective tissue—to begin forming here, requiring less bone to be resorbed to make room for attachment on the lateral surface of the implant fixture. Platform switching has been shown to have the potential to reduce the vertical bone resorption by as much as 70%.
119:, it was found that these implants exhibited less-than-expected initial crestal bone loss—the effect of bone modeling at the crest of the alveolar bone into which dental implants are placed—during healing. Several early clinical reports demonstrated enhanced soft (
312:
aspect of the buccal plate, it will be obliterated for a vertical distance of approximately 1.5-2 mm by the formation of the biologic width on the body of the implant fixture, which can lead to complications related to esthetics and long-term maintenance.
114:
The introduction of wide-diameter dental implants in the late 1980s created a situation in which mismatched standard-diameter abutments were used simply because of the lack of commercial availability of components to match the wide-diameter implants.
321:
Because the abutment is narrower in diameter than the implant fixture, a certain amount of the implant platform is exposed when an implant is platform switched, and this exposed area of the platform can allow for the tissues of the biologic width --
291:
Increased loss of inter-implant bone in the vertical dimension due to this overlap of horizontal components of the adjacent implants' biologic width can have ramifications in the anterior esthetic zone because it decreases bony support for the
287:
et al. in 2000 in a study that demonstrated that the distance between the most coronal aspect of the inter-implant bone and an imaginary line drawn between the implant platforms was greater when adjacent implants were placed ≤3 mm apart.
159:
when the implant-abutment diameter mismatch was greater than 0.8 mm, providing a 0.4 mm circumferential width of platform switch when the center of the abutment is aligned with and fixed to the center of the implant.
309:
305:
230:
213:
60:. The concept refers to placing screwed or friction fit restorative abutments of narrower diameter on implants of wider diameter, rather than placing abutments of similar diameters, referred to as
304:
Another clinical example in which the horizontal extent of crestal bone loss due to biologic width formation can negatively affect the peri-implant bony architecture is a situation in which the
229:
Recently, the lateral extent of this vertical bone loss around implants has been investigated—in other words, the thickness of bone loss that exists as a halo around the implant at its most
308:
plate of the alveolar process is very thin and lies wholly or substantially within the halo of the horizontal component of the biologic width. If an implant is placed within 1.5 mm of the
106:, a narrower abutment diameter for a given implant platform diameter is used; for example, a 4.8 mm-wide implant may be restored with a 3.8 mm-wide or 4.2 mm-wide abutment.
127:) tissue responses to these platform switched implants, leading many implant companies to incorporate platform switching into their implant systems even for narrower-body implants.
447:
Biologic width around titanium implants: a histometric analysis of the implanto-gingival junction around unloaded and loaded non-submerged implants in the canine mandible
221:
in the diagram at right) diminishes the bone-to-implant contact, contributing to a potential decrease in long-term biomechanical stability and has been well researched.
95:
of the abutment matched the diameter of the implant platform; for example, a 4.8 mm-wide abutment was placed on a 4.8 mm-wide implant—this can be termed
481:
Crestal bone changes around titanium implants: a radiographic evaluation of unloaded non-submerged and submerged implants in the canine mandible
296:
between implants. By platform switching, implants can be placed closer to teeth and to each other while maintaining more crestal bone.
212:
Around implants, biologic width formation has classically led to about 1.5 - 2 mm of bone loss in the vertical dimension at the
36:(it shares the same 5.0 mm diameter as the implant platform), while the healing abutment on the more anterior implant is
283:
biologic width serves to increase the effective vertical crestal bone loss between the implants. This was first reported by
336:
the microgap of the implant-abutment junction on the bone, allowing for a reduction in the horizontal extent of bone loss.
503:
The effect of interimplant distance on the height of the interimplant bone crest when using platform-switched implants
583:
156:
137:
430:
Platform switching for marginal bone preservation around dental implants: A systematic review and meta-analysis
151:
In line with the supposed mechanism of action, it is not merely the introduction of a platform switch, but the
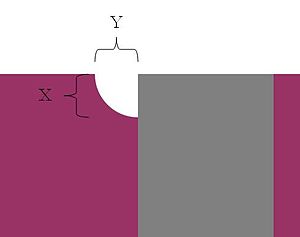
176:, while Y indicates the horizontal component of the biologic width. (Legend: Bone is purple, implant is gray)
168:
396:
Platform switching: A new concept in implant dentistry for controlling postoperative crestal bone levels
323:
293:
155:
of the implant-abutment diameter mismatch, that makes a difference. Difference in bone levels became
357:
Platform switching and marginal bone-level alterations: The results of a randomized-controlled trial
21:
206:
144:
81:
32:
placed into the lower right mandible. The healing abutment on the more posterior implant is
185:
Very much like teeth, implants exposed to the oral cavity exhibit what is known as a minimum
77:
198:
561:
Benefits of an implant platform modification technique to reduce crestal bone resorption
374:
A new implant design for crestal bone preservation: Initial observations and case report
194:
186:
173:
57:
29:
577:
284:
190:
124:
53:
141:
527:
The effect of inter-implant distance on the height of the inter-implant bone crest
241:
in the diagram at right), and research reveals that it is approximately 1.4 mm.
116:
202:
16:
189:. Biologic width is the minimum thickness of soft tissue that envelops the
45:
245:
Horizontal component affecting crestal bone loss between adjacent implants
92:
120:
85:
413:
Different types of inflammatory reactions in peri-implant soft tissues
300:
Horizontal component affecting buccal plate in narrow alveolar crests
25:
76:
After being placed in a surgical procedure, dental implants undergo
167:
15:
331:
Platform switching and the horizontal component of biologic width
140:(IAJ). A number of investigators have zeroed in on the proposed
464:
Dimensions and relations of the dentogingival junction in humans
251:
Crestal bone height as a function of distance between implants.
317:
Platform switching and the vertical component of biologic width
88:, etc.) to be cemented on, screwed down or otherwise attached.
544:
Treatment planning implant dentistry with a 2 mm twist drill
197:
are placed, and has classically been described as having a
8:
172:X indicates the vertical dimension known as
24:displays two identical 5.0 mm diameter
235:horizontal component of the biologic width
521:
519:
517:
515:
390:
388:
386:
351:
349:
148:within the width of the platform switch.
249:
345:
225:Horizontal component of biologic width
40:(it possesses a 4.1 mm diameter).
497:
495:
493:
7:
205:and 1.07 mm of underlying soft
193:that surrounds teeth and into which
14:
201:of 2.04 mm: 0.97 mm of
233:aspect—and has been termed the
1:
52:is a method used to preserve
501:Rodríguez-Ciurana X, et al.
600:
378:Pract Proceed Aesthet Dent
195:endosseous dental implants
256:Distance between implants
157:statistically significant
138:implant-abutment junction
68:peri-implant bone loss.
361:Clin Oral Implants Res
272:>3 mm apart (n=11)
177:
41:
559:Vela-Nebot X, et al.
542:Greenstein G, et al.
507:Int J Perio Rest Dent
400:Int J Perio Rest Dent
372:Baumgarten H, et al.
324:junctional epithelium
294:interproximal papilla
171:
19:
462:Gargiulo AW, et al.
479:Hermann JS, et al.
445:Cochran DL, et al.
411:Ericsson I, et al.
394:Lazzara RJ, et al.
264:≤3 mm apart (n=25)
252:
525:Tarnow DP, et al.
487:1997;68:1117-1130.
436:2010;81:1350-1366.
355:Canullo L, et al.
250:
178:
136:morphology of the
104:platform switching
91:Historically, the
50:platform switching
42:
428:Atieh MA, et al.
279:
278:
207:connective tissue
164:Proposed benefits
97:platform-matching
62:platform matching
38:platform switched
22:dental radiograph
591:
584:Prosthodontology
568:
567:2006;15:313–320.
557:
551:
540:
534:
533:2000;71:546-549.
523:
510:
509:2009;29:141–151.
499:
488:
477:
471:
470:1961;32:261-267.
460:
454:
453:1997;68:186-198.
443:
437:
426:
420:
419:1995;22:255-261.
409:
403:
392:
381:
380:2005;17:735-740.
370:
364:
363:2010;21:115-121.
353:
253:
78:osseointegration
34:platform matched
599:
598:
594:
593:
592:
590:
589:
588:
574:
573:
572:
571:
558:
554:
550:2010;31(2):2-10
541:
537:
524:
513:
500:
491:
478:
474:
461:
457:
444:
440:
427:
423:
410:
406:
393:
384:
371:
367:
354:
347:
342:
333:
319:
302:
280:
247:
227:
183:
166:
133:
117:Serendipitously
112:
74:
58:dental implants
30:dental implants
12:
11:
5:
597:
595:
587:
586:
576:
575:
570:
569:
552:
535:
511:
489:
472:
455:
438:
421:
404:
382:
365:
344:
343:
341:
338:
332:
329:
318:
315:
301:
298:
277:
276:
273:
269:
268:
265:
261:
260:
257:
248:
246:
243:
226:
223:
187:biologic width
182:
181:Biologic width
179:
174:biologic width
165:
162:
132:
129:
111:
108:
73:
70:
56:levels around
13:
10:
9:
6:
4:
3:
2:
596:
585:
582:
581:
579:
566:
562:
556:
553:
549:
545:
539:
536:
532:
528:
522:
520:
518:
516:
512:
508:
504:
498:
496:
494:
490:
486:
482:
476:
473:
469:
465:
459:
456:
452:
448:
442:
439:
435:
431:
425:
422:
418:
414:
408:
405:
401:
397:
391:
389:
387:
383:
379:
375:
369:
366:
362:
358:
352:
350:
346:
339:
337:
330:
328:
325:
316:
314:
311:
307:
299:
297:
295:
289:
286:
285:Dennis Tarnow
274:
271:
270:
266:
263:
262:
258:
255:
254:
244:
242:
240:
236:
232:
224:
222:
220:
215:
210:
208:
204:
200:
196:
192:
191:alveolar bone
188:
180:
175:
170:
163:
161:
158:
154:
149:
146:
143:
139:
130:
128:
126:
122:
118:
109:
107:
105:
100:
98:
94:
89:
87:
83:
79:
71:
69:
65:
63:
59:
55:
54:alveolar bone
51:
47:
39:
35:
31:
27:
23:
18:
565:Implant Dent
564:
560:
555:
547:
543:
538:
530:
526:
506:
502:
484:
480:
475:
467:
463:
458:
450:
446:
441:
433:
429:
424:
417:J Clin Perio
416:
412:
407:
402:2006;26:9-17
399:
395:
377:
373:
368:
360:
356:
334:
320:
303:
290:
281:
238:
234:
228:
218:
211:
184:
152:
150:
142:inflammatory
134:
123:) and hard (
113:
103:
101:
96:
90:
75:
66:
61:
49:
43:
37:
33:
548:Compendium
340:References
259:Bone loss
203:epithelium
153:magnitude
131:Rationale
46:dentistry
26:Biomet 3i
578:Category
275:0.45 mm
267:1.04 mm
93:diameter
86:dentures
28:tapered
531:J Perio
485:J Perio
468:J Perio
451:J Perio
434:J Perio
231:coronal
214:coronal
121:gingiva
110:History
72:Concept
310:facial
306:buccal
82:crowns
102:When
20:This
199:mean
145:cell
125:bone
44:In
580::
563:.
546:.
529:.
514:^
505:.
492:^
483:.
466:.
449:.
432:.
415:.
398:.
385:^
376:.
359:,
348:^
209:.
99:.
84:,
64:.
48:,
239:Y
237:(
219:X
Text is available under the Creative Commons Attribution-ShareAlike License. Additional terms may apply.