31:
182:
730:
Galvin, James M; Ezzell, Gary; Eisbrauch, Avraham; Yu, Cedric; Butler, Brian; Xiao, Ying; Rosen, Isaac; Rosenman, Julian; Sharpe, Michael; Xing, Lei; Xia, Ping; Lomax, Tony; Low, Daniel A; Palta, Jatinder (April 2004), "Implementing IMRT in clinical practice: a joint document of the
American Society
207:
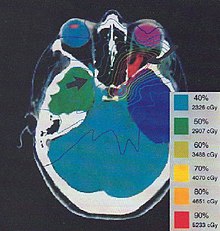
Once the treatment planner has made an initial plan, the treatment planning system calculates the required monitor units to deliver a prescribed dose to a specific area, and the distribution of dose in the body this will create. The dose distribution in the patient is dependent on the anatomy and
137:
is less commonly used and reserved for cases where specific uptake studies can enhance planning target volume delineation. Modern treatment planning systems provide tools for multimodality image matching, also known as image coregistration or fusion. Treatment simulations are used to plan the
108:
utilise inverse planning to provide further improved dose distributions (i.e. better coverage of target tumours and sparing of healthy tissue). These methods are growing in use, particularly for cancers in certain locations which have been shown to derive the greatest benefits.
235:
In inverse planning a radiation oncologist defines a patient's critical organs and tumour, after which a planner gives target doses and importance factors for each. Then, an optimisation program is run to find the treatment plan which best matches all the input criteria.
97:(MLCs) lead to 3D conformal planning (3DCRT), categorised as a Level 2 technique by the European Dynarad consortium. 3DCRT uses MLCs to shape the radiotherapy beam to closely match the shape of a target tumour, reducing the dose to healthy surrounding tissue.
277:
Thariat, Juliette; Hannoun-Levi, Jean-Michel; Sun Myint, Arthur; Vuong, Te; Gérard, Jean-Pierre (27 November 2012). "Past, present, and future of radiotherapy for the benefit of patients".
212:
of the patient allows more accurate modelling of the behaviour of the radiation as it travels through the patient's tissues. Different dose calculation models are available, including
669:
Lahanas, M; Baltas, D; Giannouli, S (7 March 2003). "Global convergence analysis of fast multiobjective gradient-based dose optimization algorithms for high-dose-rate brachytherapy".
86:
images, often by hand and with manual calculations. Computerised treatment planning systems began to be used in the 1970s to improve the accuracy and speed of dose calculations.
200:
and minimising the dose to healthy tissue. The required decisions include how many radiation beams to use, which angles each will be delivered from, whether attenuating
573:
227:
This type of planning is only sufficiently adept to handle relatively simple cases in which the tumour has a simple shape and is not near any critical organs.
435:
Intensity
Modulated Radiation Therapy Collaborative Working Group (November 2001). "Intensity-modulated radiotherapy: current status and issues of interest".
521:
AlDuhaiby, Eman Z; Breen, Stephen; Bissonnette, Jean-Pierre; Sharpe, Michael; Mayhew, Linda; Tyldesley, Scott; Wilke, Derek R; Hodgson, David C (2012).
158:
planning involves selecting the appropriate catheter positions and source dwell times (in HDR brachytherapy) or seed positions (in LDR brachytherapy).
320:
Kolitsi, Zoi; Dahl, Olav; Van Loon, Ron; Drouard, Jean; Van Dijk, Jan; Ruden, Bengt Inge; Chierego, Giorgio; Rosenwald, Jean Claude (December 1997).
143:
192:
In forward planning, the planner places beams into a radiotherapy treatment planning system that can deliver sufficient radiation to a
772:
150:), this process involves selecting the appropriate beam type (which may include photons, electrons and protons), energy (e.g. 6, 18
173:, allowing the clinician to evaluate the uniformity of the dose to the diseased tissue (tumor) and sparing of healthy structures.
572:
Society and
College of Radiographers; Institute of Physics and Engineering in Medicine; Royal College of Radiologists (2015),
575:
Radiotherapy Board - Intensity
Modulated Radiotherapy (IMRT) in the UK: Current access and predictions of future access rates
257:
186:
523:"A national survey of the availability of intensity-modulated radiation therapy and stereotactic radiosurgery in Canada"
239:
In contrast to the manual trial-and-error process of forward planning, inverse planning uses the optimiser to solve the
134:
208:
beam modifiers such as wedges, specialized collimation, field sizes, tumor depth, etc. The information from a prior
889:
130:
139:
644:
Optimization of
Catheter Position and Dwell Time in Prostate HDR Brachytherapy using HIPO and Linear Programming
894:
217:
686:
201:
138:
geometric, radiological, and dosimetric aspects of the therapy using radiation transport simulations and
170:
760:
365:
Transition from 2-D Radiotherapy to 3-D Conformal and
Intensity Modulated Radiotherapy IAEA-TECDOC-1588
678:
391:
94:
51:
691:
55:
731:
for
Therapeutic Radiology and Oncology and the American Association of Physicists in Medicine.",
712:
302:
221:
63:
363:
865:
816:
768:
744:
704:
624:
554:
503:
452:
417:
344:
322:"Quality assurance in conformal radiotherapy: DYNARAD consensus report on practice guidelines"
294:
105:
101:
39:
855:
847:
806:
798:
736:
696:
651:
614:
604:
544:
534:
493:
483:
444:
407:
399:
336:
286:
151:
30:
834:
Gintz, D; Latifi, K; Caudell, J; Nelms, B; Zhang, G; Moros, E; Feygelman, V (8 May 2016).
240:
197:
181:
118:
59:
204:
be used, and which MLC configuration will be used to shape the radiation from each beam.
17:
682:
395:
860:
835:
811:
786:
619:
592:
549:
522:
498:
471:
321:
448:
340:
883:
700:
252:
155:
67:
306:
716:
472:"Current role of modern radiotherapy techniques in the management of breast cancer"
655:
740:
802:
213:
83:
290:
593:"The Role of Imaging in Radiation Therapy Planning: Past, Present, and Future"
382:
Fraass, Benedick A. (1995). "The development of conformal radiation therapy".
851:
869:
820:
748:
708:
642:
Karabis, A; Belloti, P; Baltas, D (2009). O. Dössel; W.C. Schlegel (eds.).
628:
558:
539:
507:
488:
456:
298:
609:
421:
412:
348:
224:, with precision versus computation time being the relevant trade-off.
209:
126:
90:
403:
193:
71:
93:, more powerful computers, improved dose calculation algorithms and
133:
provides excellent secondary image set for soft tissue contouring.
591:
Pereira, Gisele C.; Traughber, Melanie; Muzic, Raymond F. (2014).
180:
29:
161:
The more formal optimization process is typically referred to as
646:. World Congress on Medical Physics and Biomedical Engineering.
147:
82:
In the early days of radiotherapy planning was performed on 2D
836:"Initial evaluation of automated treatment planning software"
437:
International
Journal of Radiation Oncology, Biology, Physics
129:
is often the primary image set for treatment planning while
66:
plan the appropriate external beam radiotherapy or internal
650:. Vol. 25, no. 1. Munich. pp. 612–615.
787:"Intensity-modulated radiotherapy - what is it?"
50:) is the process in which a team consisting of
735:, vol. 58, no. 5, pp. 1616–34,
154:(MeV) photons) and physical arrangements. In
8:
371:, Vienna: International Atomic Energy Agency
840:Journal of Applied Clinical Medical Physics
169:. Plans are often assessed with the aid of
34:Doctor reviewing a radiation treatment plan
859:
810:
690:
618:
608:
548:
538:
497:
487:
411:
125:for a computer-aided design procedure. A
269:
70:treatment technique for a patient with
144:intensity modulated radiation therapy
7:
763:, Ibbott G. and Hendee E. (2005).
476:World Journal of Clinical Oncology
25:
279:Nature Reviews Clinical Oncology
671:Physics in Medicine and Biology
258:Image-guided radiation therapy
1:
733:Int J Radiat Oncol Biol Phys.
656:10.1007/978-3-642-03474-9_172
597:BioMed Research International
449:10.1016/S0360-3016(01)01749-7
341:10.1016/S0167-8140(97)00144-8
187:Optic nerve sheath meningioma
27:In cancer or tumor treatments
741:10.1016/j.ijrobp.2003.12.008
196:while both sparing critical
135:Positron emission tomography
44:radiation treatment planning
803:10.1102/1470-7330.2004.0003
100:Level 3 techniques such as
911:
701:10.1088/0031-9155/48/5/304
291:10.1038/nrclinonc.2012.203
243:as set up by the planner.
131:magnetic resonance imaging
765:Radiation Therapy Physics
329:Radiotherapy and Oncology
218:convolution-superposition
18:Treatment Planning System
852:10.1120/jacmp.v17i3.6167
470:Ozyigit, Gokhan (2014).
540:10.1186/1748-717X-7-18
489:10.5306/wjco.v5.i3.425
253:Brachytherapy planning
222:monte carlo simulation
189:
185:Treatment plan for an
171:dose-volume histograms
35:
184:
113:Image guided planning
95:Multileaf collimators
52:radiation oncologists
33:
64:medical dosimetrists
785:Taylor, A. (2004).
767:. Wiley-Liss Publ.
683:2003PMB....48..599L
610:10.1155/2014/231090
396:1995MedPh..22.1911F
56:radiation therapist
527:Radiation Oncology
190:
121:is used to form a
60:medical physicists
36:
890:Radiation therapy
648:IFMBE Proceedings
390:(11): 1911–1921.
16:(Redirected from
902:
874:
873:
863:
831:
825:
824:
814:
782:
776:
758:
752:
751:
727:
721:
720:
694:
666:
660:
659:
639:
633:
632:
622:
612:
588:
582:
581:
580:
569:
563:
562:
552:
542:
518:
512:
511:
501:
491:
467:
461:
460:
432:
426:
425:
415:
404:10.1118/1.597446
379:
373:
372:
370:
359:
353:
352:
326:
317:
311:
310:
274:
231:Inverse planning
177:Forward planning
167:inverse planning
163:forward planning
152:megaelectronvolt
21:
910:
909:
905:
904:
903:
901:
900:
899:
895:Medical physics
880:
879:
878:
877:
833:
832:
828:
784:
783:
779:
759:
755:
729:
728:
724:
668:
667:
663:
641:
640:
636:
590:
589:
585:
578:
571:
570:
566:
520:
519:
515:
469:
468:
464:
434:
433:
429:
384:Medical Physics
381:
380:
376:
368:
361:
360:
356:
324:
319:
318:
314:
276:
275:
271:
266:
249:
241:Inverse Problem
233:
179:
123:virtual patient
119:medical imaging
115:
80:
28:
23:
22:
15:
12:
11:
5:
908:
906:
898:
897:
892:
882:
881:
876:
875:
846:(3): 331–346.
826:
791:Cancer Imaging
777:
753:
722:
692:10.1.1.20.2302
677:(5): 599–617.
661:
634:
583:
564:
513:
462:
443:(4): 880–914.
427:
413:2027.42/134769
374:
354:
335:(3): 217–223.
312:
268:
267:
265:
262:
261:
260:
255:
248:
245:
232:
229:
178:
175:
114:
111:
79:
76:
26:
24:
14:
13:
10:
9:
6:
4:
3:
2:
907:
896:
893:
891:
888:
887:
885:
871:
867:
862:
857:
853:
849:
845:
841:
837:
830:
827:
822:
818:
813:
808:
804:
800:
796:
792:
788:
781:
778:
774:
773:0-471-39493-9
770:
766:
762:
757:
754:
750:
746:
742:
738:
734:
726:
723:
718:
714:
710:
706:
702:
698:
693:
688:
684:
680:
676:
672:
665:
662:
657:
653:
649:
645:
638:
635:
630:
626:
621:
616:
611:
606:
602:
598:
594:
587:
584:
577:
576:
568:
565:
560:
556:
551:
546:
541:
536:
532:
528:
524:
517:
514:
509:
505:
500:
495:
490:
485:
482:(3): 425–39.
481:
477:
473:
466:
463:
458:
454:
450:
446:
442:
438:
431:
428:
423:
419:
414:
409:
405:
401:
397:
393:
389:
385:
378:
375:
367:
366:
362:IAEA (2008),
358:
355:
350:
346:
342:
338:
334:
330:
323:
316:
313:
308:
304:
300:
296:
292:
288:
284:
280:
273:
270:
263:
259:
256:
254:
251:
250:
246:
244:
242:
237:
230:
228:
225:
223:
219:
215:
211:
205:
203:
199:
195:
188:
183:
176:
174:
172:
168:
164:
159:
157:
156:brachytherapy
153:
149:
145:
141:
136:
132:
128:
124:
120:
112:
110:
107:
103:
98:
96:
92:
89:By the 1990s
87:
85:
77:
75:
73:
69:
68:brachytherapy
65:
61:
57:
53:
49:
45:
41:
32:
19:
843:
839:
829:
797:(2): 68–73.
794:
790:
780:
764:
756:
732:
725:
674:
670:
664:
647:
643:
637:
600:
596:
586:
574:
567:
530:
526:
516:
479:
475:
465:
440:
436:
430:
387:
383:
377:
364:
357:
332:
328:
315:
285:(1): 52–60.
282:
278:
272:
238:
234:
226:
206:
191:
166:
162:
160:
140:optimization
122:
116:
99:
88:
81:
47:
43:
40:radiotherapy
37:
214:pencil beam
117:Typically,
884:Categories
603:: 231090.
264:References
761:Hendee W.
687:CiteSeerX
533:(1): 18.
870:27167292
821:18250011
749:15050343
709:12696798
629:24812609
559:22309806
508:25114857
457:11704310
307:16206956
299:23183635
247:See also
91:CT scans
861:5690942
812:1434586
717:2382119
679:Bibcode
620:4000658
550:3339388
499:4127613
422:8587545
392:Bibcode
349:9426115
210:CT scan
127:CT scan
78:History
868:
858:
819:
809:
771:
747:
715:
707:
689:
627:
617:
557:
547:
506:
496:
455:
420:
347:
305:
297:
202:wedges
198:organs
194:tumour
142:. For
72:cancer
713:S2CID
579:(PDF)
369:(PDF)
325:(PDF)
303:S2CID
84:x-ray
866:PMID
817:PMID
769:ISBN
745:PMID
705:PMID
625:PMID
601:2014
555:PMID
504:PMID
453:PMID
418:PMID
345:PMID
295:PMID
220:and
165:and
148:IMRT
106:VMAT
104:and
102:IMRT
62:and
856:PMC
848:doi
807:PMC
799:doi
737:doi
697:doi
652:doi
615:PMC
605:doi
545:PMC
535:doi
494:PMC
484:doi
445:doi
408:hdl
400:doi
337:doi
287:doi
48:RTP
38:In
886::
864:.
854:.
844:17
842:.
838:.
815:.
805:.
793:.
789:.
743:,
711:.
703:.
695:.
685:.
675:48
673:.
623:.
613:.
599:.
595:.
553:.
543:.
529:.
525:.
502:.
492:.
478:.
474:.
451:.
441:51
439:.
416:.
406:.
398:.
388:22
386:.
343:.
333:45
331:.
327:.
301:.
293:.
283:10
281:.
216:,
74:.
58:,
54:,
42:,
872:.
850::
823:.
801::
795:4
775:.
739::
719:.
699::
681::
658:.
654::
631:.
607::
561:.
537::
531:7
510:.
486::
480:5
459:.
447::
424:.
410::
402::
394::
351:.
339::
309:.
289::
146:(
46:(
20:)
Text is available under the Creative Commons Attribution-ShareAlike License. Additional terms may apply.